SKIN PROBLEMS/
Psoriasis
Understanding Psoriasis: Symptoms, Causes, And Effective Treatment Options
Psoriasis is a chronic skin disease that is characterised by symmetrically distributed red scaly plaques.

Introduction To Psoriasis: Understanding The Basics And Symptoms
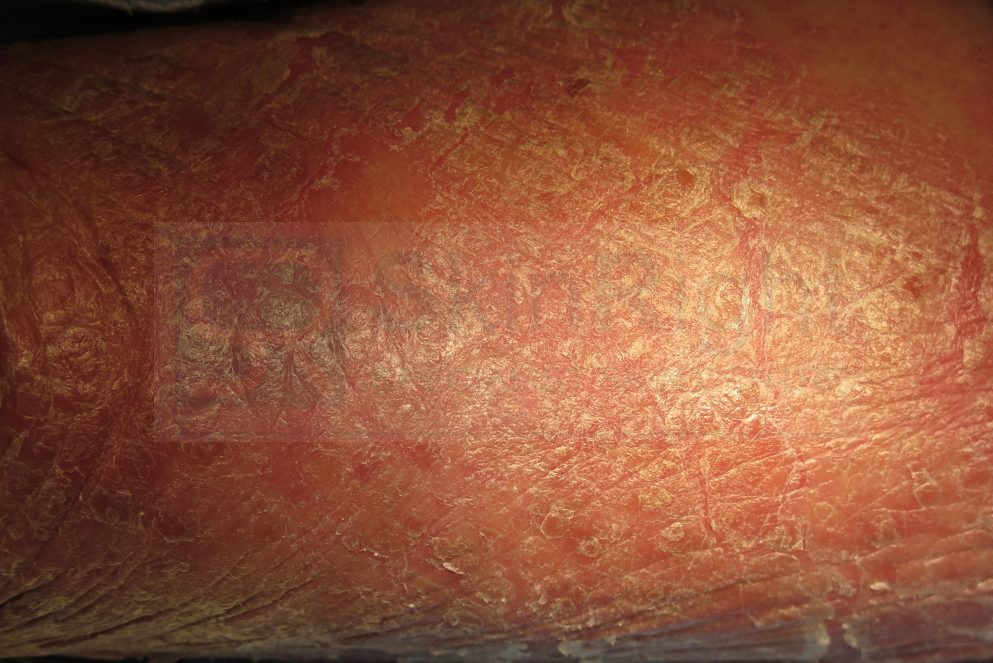
Psoriasis is a chronic autoimmune condition that manifests primarily on the skin but can also affect joints, causing a condition known as psoriatic arthritis. It occurs when the immune system erroneously accelerates the growth cycle of skin cells, leading to the rapid buildup of cells on the skin’s surface. This results in thick, red, scaly patches that can be itchy and sometimes painful.
While the exact cause of psoriasis is not fully understood, it is believed to involve a combination of genetic predispositions and environmental factors. Common triggers may include stress, infections, and certain medications. Understanding the symptoms is crucial for early diagnosis and effective management. Symptoms can vary widely, but the most recognizable signs include red patches of skin covered with silvery scales, dry and cracked skin that may bleed, itching, burning sensations, and nails that become thickened or ridged.
Psoriasis can appear anywhere on the body, although it is most commonly found on the scalp, elbows, and knees. Recognizing and understanding these symptoms is the first step in managing this complex condition.
Related Video
Exploring The Causes And Triggers Of Psoriasis
Psoriasis is a complex autoimmune condition that remains under extensive study to fully understand its causes and triggers. At its core, psoriasis results from an overactive immune system that speeds up the life cycle of skin cells, leading to the buildup of scales and red patches. Genetics plays a significant role, as psoriasis often runs in families, indicating a strong hereditary component.
However, environmental factors can also act as triggers, including stress, which heightens the immune response, and skin injuries, such as cuts or sunburns, which can exacerbate symptoms. Infections, particularly those caused by streptococcal bacteria, have been linked to the onset of certain types of psoriasis. Additionally, lifestyle factors like smoking, excessive alcohol consumption, and obesity are known to increase the risk of flare-ups, making them important contributors to the condition.
Traditional Treatment Options: The Role Of Corticosteroids
Corticosteroids have long played a central role in the traditional treatment regimen for managing psoriasis. These medications are highly effective in reducing the inflammation and immune response associated with psoriasis, helping to control the rapid proliferation of skin cells that characterizes the condition. Topical corticosteroids are the most commonly used form in psoriasis treatment and are available in varying strengths, from mild to potent, allowing healthcare providers to tailor treatment to the severity and location of the psoriasis lesions.
Mild corticosteroids may be sufficient for treating sensitive areas such as the face or for use in children, while stronger formulations are often necessary for thicker plaques typically found on the elbows, knees, and scalp. When applied, these medications work by penetrating the skin and interrupting the inflammatory pathways, thereby alleviating redness, swelling, itching, and scaling. The therapeutic benefits of corticosteroids can lead to significant improvements in quality of life for individuals struggling with psoriasis.
Despite their efficacy, the prolonged use of corticosteroids must be approached with caution due to potential side effects. Long-term application, particularly of high-potency corticosteroids, can lead to skin thinning, stretch marks, and systemic absorption which may affect adrenal gland function.
Overall, while corticosteroids remain a cornerstone in the traditional management of psoriasis, their use requires careful balancing to maximize benefits and minimize potential adverse effects. Through judicious application and monitoring, corticosteroids can effectively help those with psoriasis achieve relief from their symptoms and a better quality of life.
The Use Of Methotrexate In Managing Psoriasis Symptoms
Methotrexate is a well-established systemic medication used in the management of moderate to severe psoriasis, particularly when topical treatments is insufficient. Originally developed as a chemotherapy agent, methotrexate works by inhibiting the metabolism of folic acid, which plays a crucial role in the rapid proliferation of skin cells and the immune response that contributes to psoriasis symptoms. By slowing down cell growth and suppressing immune system activity, methotrexate helps reduce the frequency and severity of psoriatic flare-ups, leading to clearer skin and relief from itching and discomfort.
The efficacy of methotrexate in treating psoriasis arises from its impact on rapidly dividing cells, such as the keratinocytes in psoriatic plaques. Patients often observe a substantial reduction in the scaling, redness, and thickness of the affected skin. Additionally, methotrexate is beneficial in managing psoriatic arthritis, a condition that often accompanies psoriasis and causes joint pain and swelling. The dual advantage of addressing both skin and joint symptoms makes methotrexate a preferred choice for individuals suffering from both forms of the disease.
However, methotrexate treatment requires careful monitoring due to potential side effects, particularly pertaining to liver function and blood cell counts. Regular blood tests are essential to ensure that the liver remains healthy and that bone marrow suppression does not occur. Physicians often prescribe folic acid supplements to mitigate some of these side effects. Despite the necessity for monitoring, methotrexate remains a cornerstone in the multifaceted approach to psoriasis treatment, offering significant relief to many patients and improving their quality of life.
Advanced Treatment: The Emergence Of BiologicsAdvanced Treatment: The Emergence Of Biologics
Biologics represent a groundbreaking class of drugs in the treatment of psoriasis, fundamentally different from traditional systemic medications. Derived from living organisms, these drugs are designed to target specific components of the immune system. While traditional systemic treatments, such as methotrexate or cyclosporine, suppress the immune system more broadly, biologics focus on precise molecules involved in the inflammatory pathway, thereby tackling psoriasis at its root.
These medications work by inhibiting the activity of particular cytokines, proteins crucial to the inflammatory processes underlying psoriasis. Key targets include tumor necrosis factor-alpha (TNF-α), interleukin-12 (IL-12), interleukin-23 (IL-23), and interleukin-17 (IL-17). By impeding these molecules, biologics reduce the inflammatory response that triggers the excessive production of skin cells, effectively managing the condition’s severity.
The introduction of biologics has significantly improved the quality of life for many individuals with psoriasis. Patients who once struggled with limited treatment results have found biologics to be remarkably effective, often achieving clear or almost clear skin within months of initiation. Moreover, the specificity of biologics translates to fewer side effects compared to traditional therapies. The risk of systemic effects is reduced, as biologics do not broadly suppress the immune system, making them a safer long-term option for many patients.
Related Video
Existing patient information
Please Contact Us for Password @ 26111006
如果你要將以下嘅內容隱藏,可以在Inner section的Advanced tab裏面的CSS ID欄位上填上 hiddenSection
銀屑病/牛皮癬知識